Managed care programs help millions of Americans access affordable healthcare, but they also create opportunities for fraud and abuse. Detecting fraudulent patterns early protects both your brokerage and the clients you represent. Watch for unusual billing patterns, falsified claims, or discrepancies in provider documentation that signal unethical or illegal activity.
According to the University of Virginia, healthcare fraud costs the United States over $100 billion annually. That staggering figure underscores how critical it is to stay alert to deception within managed care operations.
Whether you lead a small brokerage or oversee large-scale insurance accounts, understanding warning signs and applying targeted prevention techniques keeps your business compliant, credible, and trusted.
What Are the Key Red Flags in Managed Care Fraud?
Fraud in managed care programs often hides behind routine paperwork or claims activity. Red flags in insurance can appear subtle, such as identical billing patterns or mismatched treatment codes, but they reveal deeper issues when tracked over time.
The biggest red flags include inconsistent patient records, unusually high reimbursement requests, and repetitive procedures billed under different codes. Other red flags include:
- Suspicious provider relationships
- Vague documentation
- Identical claims across patients
- Unnecessary medical tests
Train your team to question data patterns that don’t make logical or financial sense. Early awareness can prevent an investigation before it starts.
How Can Brokerages Identify Fraudulent Provider Behavior?
Brokers often stand between clients and insurers, making them the first line of defense against managed care fraud. Detecting provider abuse requires a careful review of data and pattern analysis.
Monitoring claim frequency, treatment types, and provider clusters is one of the most effective brokerage defense strategies. Compare patient volume with service billing trends, and watch for sudden increases in specialized procedures or non-covered services.
Establish automated audit alerts within your systems and maintain direct communication with your insurers when something appears off. Cooperation between brokers, carriers, and investigators builds accountability throughout the network.
What Are the Most Common Insurance Fraud Indicators?
Fraud indicators appear across both provider and brokerage levels. Some of the most common seguro fraud indicators include:
- Billing for services not rendered
- Falsified patient signatures
- Unlicensed or suspended providers
- Altered medical documentation
Strong internal controls make it harder for fraud to infiltrate your brokerage’s daily operations. Require dual authorization for large claims, review suspicious reimbursements manually, and ensure every document submitted has a verifiable source.
Fraudsters often rely on the assumption that busy offices won’t notice inconsistencies. Make sure yours does.
How Can Brokerages Build Effective Internal Controls?
Protecting your organization requires structure and vigilance. Strong internal protocols minimize risk and stop fraud before it escalates.
Create written policies outlining verification steps for every claim, along with consistent staff training on identifying red flags. Practical steps include:
- Verifying all provider credentials
- Maintaining secure data access
- Recording all client communications
- Reviewing high-value claims manually
When your internal checks are clear and consistent, your brokerage can respond faster and more confidently to suspicious activity.
What Role Does Data Analytics Play in Detecting Fraud?
Advanced analytics help brokers spot anomalies that humans may overlook. Software that identifies irregular billing codes, duplicate claims, or sudden spikes in reimbursements can signal early fraud attempts.
Use data analysis tools to cross-check provider activity against regional and historical averages. When patterns diverge significantly, initiate review protocols.
Data visualization dashboards, combined with human oversight, empower teams to focus investigations on the most suspicious behaviors without overloading compliance staff.
How Can You Prevent Managed Care Fraud Before It Starts?
Prevention always costs less than recovery. The most successful fraud-prevention programs combine proactive training, policy enforcement, and continuous evaluation.
Focus your team’s efforts on transparency, traceability, and accountability to reduce exposure to fraudulent claims.
Regularly educate employees on preventing managed care fraud through updated case studies, audits, and open communication with legal counsel. Encourage whistleblowing in a protected, confidential environment. Fraud often surfaces first from within your own network.
Why Should Brokerages Partner With Whistleblower Attorneys?
Even the most diligent brokerages can face exposure when fraud occurs elsewhere in the chain. Partnering with whistleblower and fraud attorneys provides expert defense and protection.
Legal partners experienced in managed care investigations can guide you through reporting, compliance, and defense if your brokerage becomes involved in a claim.
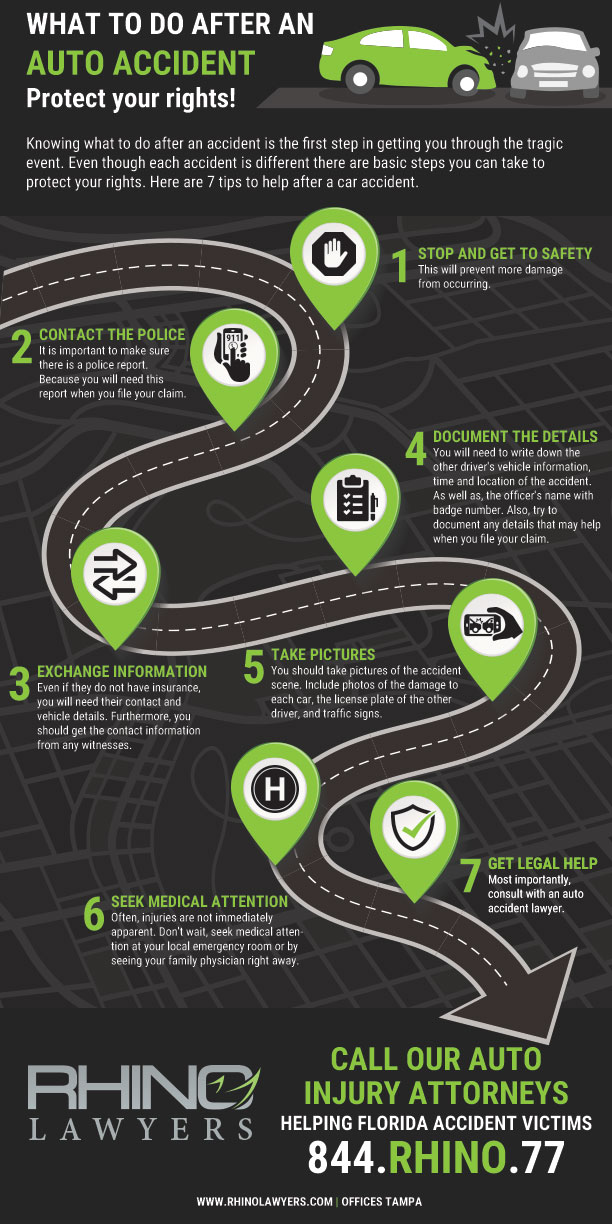
They can also represent you if an internal report leads to retaliation or regulatory scrutiny. Firms like RHINO Lawyers, with their whistleblower advocacy and insurance defense experience, help safeguard your reputation while ensuring justice for legitimate claims.
Preguntas frecuentes
What Is Managed Care Fraud?
Managed care fraud occurs when healthcare providers, brokers, or insurers intentionally misrepresent services or costs to gain a financial advantage. Examples include inflated billing, false claims, and unnecessary procedures.
Who Investigates Managed Care Fraud?
Federal agencies such as the FBI, the Office of Inspector General (OIG), and state fraud bureaus handle investigations. They often collaborate with private brokers, attorneys, and insurance carriers.
What Are the Legal Penalties for Managed Care Fraud?
Penalties may include heavy fines, restitution, or prison time under the False Claims Act. Civil penalties can also apply to organizations that fail to prevent or report known fraud.
How Can Brokers Strengthen Brokerage Defense Strategies?
Brokers should develop written compliance programs, assign a dedicated fraud officer, and maintain open communication with insurers. Regular audits and risk assessments build lasting credibility.
What Are Some Early Red Flags in Insurance That Brokers Overlook?
Commonly missed signs include duplicate claims, mismatched patient details, and sudden billing changes from trusted providers. Reviewing these regularly can prevent costly exposure.
How Does Technology Help in Detecting Managed Care Fraud?
Automation tools can scan thousands of claims for irregularities in seconds. These systems learn patterns over time, helping detect new and evolving schemes that might otherwise go unnoticed.
Protecting Your Brokerage From Fraud
Fraud detection is no longer optional; it’s essential. Brokers must balance growth and compliance while protecting clients and insurers alike. Strong systems, transparent policies, and trusted legal support form your best defense.
Managed care may be complex, but vigilance and proactive monitoring keep your brokerage protected from risk and liability.
En RHINO Lawyers, we help clients identify fraudulent activity, report wrongdoing, and defend against claims with bold legal representation. Whether you suspect wrongdoing within your network or face an ongoing investigation, our team will safeguard your business and reputation.
CONTACTO RHINO Lawyers today for a confidential case evaluation and exceptional guidance on navigating managed care fraud detection and prevention.