Enrollment and disenrollment fraud is one of the most common problems inside managed care organizations, and it affects patients, public programs, and taxpayers. This type of misconduct happens when people are added to or removed from health plans without proper consent or documentation. It creates gaps in care, inflates costs, and undermines fraud prevention in healthcare.
Many of these cases only come to light because someone inside the system notices signs of wrongdoing. Workers may see forged signatures, unusual enrollment spikes, or complaints from patients who never agreed to join a plan. When this happens, speaking up is important.
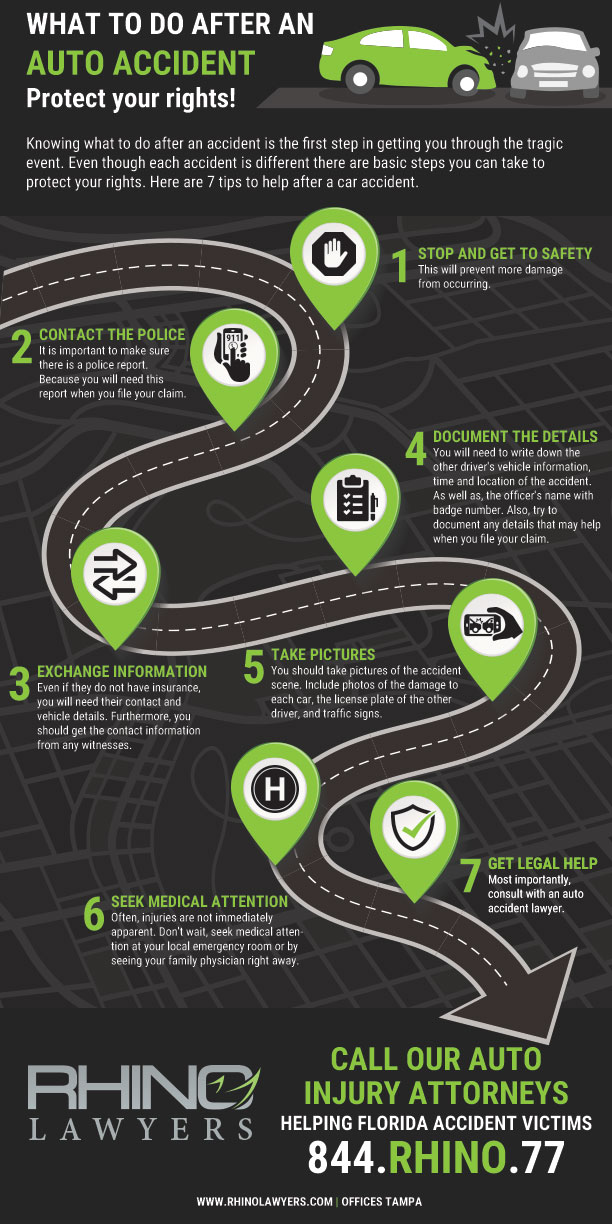
With the right legal support, whistleblowers can protect themselves, expose wrongdoing, and help keep healthcare programs honest and reliable. In this blog post, RHINO Lawyers will explain how enrollment and disenrollment fraud happens, why it harms patients and programs, and how whistleblowers can take action with strong legal protection.
What Enrollment Fraud Looks Like
Enrollment fraud happens when people are added to health plans without clear consent. Some workers may use forged signatures or rush forms through without real approval. Others may enroll people who are not eligible.
Many cases begin with small steps that grow over time. For example, a worker may be pushed to meet quotas or targets, and patients may report coverage they never asked for.
Insiders often notice patterns first, such as sudden spikes in new members or repeated complaints from confused patients.
What Disenrollment Fraud Looks Like
Disenrollment fraud occurs when people are removed from health plans without proper notice. Some workers may drop high-cost patients to improve performance metrics, while others may cancel coverage to shift someone into another plan.
Patients often discover the issue when a doctor visit or medication is denied. Workers may see sudden drops in membership. Care disruptions, surprise bills, and missed treatments are common signs that something is wrong.
Why This Type of Fraud Happens
Fraud often grows from pressure to meet enrollment goals or improve financial results. Workers may be judged on numbers, not accuracy.
Poor oversight also creates space for misconduct, and weak checks, rushed procedures, and unclear policies allow fraud to slip through.
Some groups cut corners to gain bonuses, reduce expenses, or secure contracts. Strong oversight reduces these incentives.
Warning Signs for Workers and Insiders
Unusual enrollment spikes, repeated complaints, and forged or incomplete paperwork are early warnings. Workers may also receive pressure to enroll or remove people quickly.
Missing consent forms, altered documents, or sudden shifts in membership counts often signal deeper issues. A rise in patient confusion or claims denials can also point toward enrollment or disenrollment misconduct.
How Fraud Affects Patients and Public Programs
Patients can lose access to doctors, face surprise bills, or miss needed care, while families may struggle to fix coverage changes they never agreed to.
Public programs face higher costs due to false enrollments and unstable membership. Fraud also harms trust in managed care systems. Taxpayer funds are stretched, and oversight agencies must spend time correcting errors that should never have occurred.
How Whistleblowers Help Expose Enrollment and Disenrollment Fraud
Whistleblowers provide details that internal records alone cannot reveal, as they understand:
- Workflows
- Documents
- Patrones
Reports from insiders often give investigators a clear view of how fraud operates. By stepping forward, whistleblowers protect patients, strengthen oversight, and help recover public funds that were misused.
Key Laws That Protect Whistleblowers
El Ley de reclamaciones falsas allows people to report fraud against federal programs and seek financial rewards when funds are recovered. The Anti-Kickback Statute and Stark Law also support people who expose illegal practices in healthcare settings.
Workers who speak up gain protection from retaliation, including unfair treatment, firing, or harassment. Strong legal support helps whistleblowers act safely.
Why RHINO Lawyers Is a Strong Option for Whistleblowers
Aquí en RHINO Lawyers, we focus on protecting people who uncover wrongdoing in healthcare settings. Clients work directly with our experienced attorneys who handle fraud cases daily.
Our team offers confidential guidance, clear communication, and steady support from start to finish. Whistleblowers also receive help with retaliation issues and potential financial recovery. RHINO Lawyers stands with workers who choose to do the right thing.
Preguntas frecuentes
How Can Patients Tell if Their Coverage Was Changed Without Consent?
Patients often notice unexpected mail, unfamiliar plan names, or new ID cards they never requested. Confusion during doctor visits or sudden issues with prescriptions can also reveal unauthorized changes in coverage.
Do Workers Risk Anything by Reporting Enrollment or Disenrollment Misconduct?
Workers may worry about retaliation, yet federal laws offer strong safeguards. Our team at RHINO Lawyers helps protect their rights, guide them through the process, and reduce the stress of coming forward.
Can Enrollment or Disenrollment Fraud Happen Through Phone or Online Sign-Ups?
Fraud can occur through rushed phone calls, misrepresented online forms, or digital entries made without informed consent. Electronic systems make tracking easier, but they can also hide improper actions when oversight is weak.
Are Patients Ever Asked to Approve Changes They Don’t Fully Understand?
Some patients are shown quick explanations or pressured to sign forms with limited detail. Misleading summaries or incomplete disclosures can lead to coverage changes that patients never intended to authorize.
How Do These Schemes Create Financial Risks for Public Programs?
Fraud leads to inflated membership counts, unstable enrollment levels, and incorrect payments that drain public funds. Program administrators must redirect time and resources to repair errors caused by fraudulent activity.
Why Should Insiders Choose RHINO Lawyers When Reporting Fraud?
RHINO Lawyers provides confidential, experienced support for people who want to expose wrongdoing and protect patients. Our team helps whistleblowers understand their rights, navigate next steps, and build a strong, protected case.
Understanding Fraud in Managed Care Organizations
The bottom line is that healthcare programs work best when people are treated honestly, yet managed care organizations can fall into harmful practices that disrupt care and waste public funds. Workers and patients who notice problems play a key role in identifying fraud in managed care, especially in cases involving healthcare enrollment fraud or improper removals from coverage.
RHINO Lawyers guides whistleblowers through every step with confidential support and strong legal protection. Contacte con nuestro equipo to discuss your concerns and learn how to move forward safely.